The Controversial Birth Control That Destroys Your Body
by Amy Martyn
APR 6 2016 4:55 PM
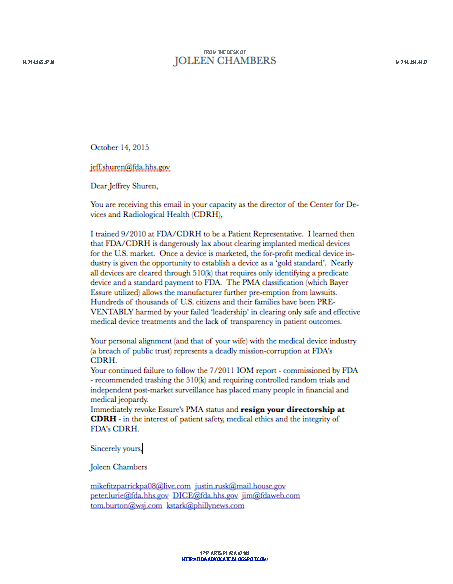
COURTESY OF BAYER
Despite thousands of women's complaints about Essure—ranging from uterus perforation to miscarriage—the FDA allows the birth control device to remain on the market. Jessica Smith describes how her Essure implant turned her body against her.
Jessica Smith's unedited, angry comment is still on the FDA's website, much to her surprise. "You had an opportunity to remove Essure from the market. You blew it," it reads. Despite complaints from women who say they've experienced painful and severe side effects such as constant cramping, still births, ectopic pregnancies, and miscarriages from the sterilization implant Essure, the Food and Drug Administration has so far allowed drug maker Bayer AG to continue to selling its product.
"Like all forms of birth control, Essure is not perfect and women may become pregnant despite use of the device," Dr. William Maisel, the FDA's Center for Devices and Radiological Health director, said in a statement. Due to multiple lawsuits regarding Essure and a recent congressional investigation, the FDA announced in February that it would place a "black box" warning on Essure and order Bayer AG to conduct more safety studies on the device.
In the meantime, as Essure remains for sale but under federal review, the FDA has invited patients to leave public comments on its website about their experience with the controversial birth control implant. "You could have allowed us the opportunity to be compensated for our horribly damaged bodies, careers, relationships and lives. But you didn't. You blew it," Jessica's post goes on. "You blew it worse than the sex workers blew your Deputy for science at the FDA Center of Devices and Radiological Health back in 2012," she ends the post, crudely referencing the 2012 arrest of the FDA's Maisel in an alleged prostitution sting.
Jessica keeps a cheerful face on, but, like other woman who complain about Essure, she is also clearly bitter. She developed a painful condition called pelvic adhesion disease, in which her reproductive system is fused to her digestive system due to scar tissue. She and her doctors believe this is a result of the Essure implant.
In an interview at her apartment in North Texas, joined by two of her close friends, Jessica showed Broadly her extensive medical records and described the chaotic process of trying to find a doctor who might be able to "fix" her.
Jessica at home
After Jessica gave birth to fifth baby in 2013, she decided to go on a more permanent form of birth control. She considered her options: She could have had her "tubes tied,"—known medically as tubal ligation, the older and more common form of female sterilization—but she decided not to because she had no guaranteed paid sick days left to recover from surgery. Essure then seemed to be the more practical choice; Bayer AG claims that, unlike tubal ligation, Essure is a not a surgery but a quick, non-invasive outpatient procedure. Jessica says her doctor told her the recovery time would be a day.
She says she felt the pain immediately as her doctor implanted the device. She remembers being told to take an Advil. "She's a really conservative doctor, so the impression I had is she thought I was being kind of a weenie," Jessica recalls.
When Jessica got home that night, she says she started passing large tissue. According to Jessica, the nurse on call "said that sounded normal and I didn't need to come back to the doctor for that. And I was like, 'If that's normal, why isn't that one of the side effects listed?'"
You had an opportunity to remove Essure from the market. You blew it worse than the sex workers blew your Deputy for science at the FDA Center of Devices and Radiological Health back in 2012.
The bleeding didn't stop. Not for 10 months. Jessica says that she felt as though she was on her period through the entire 10-month span. She felt a constant pain in her abdomen, which vacillated between feeling bearable to being so intense that she could not stand, and therefore couldn't work.
She made regular trips to the emergency room. Doctors at the E.R. diagnosed her with vague conditions like "abdominal pain" and told her to return to her implanting physician. "I would hang my hat that you have an STD," she remembers one doctor telling her.
Another told her she was suffering from the "period from hell" and prescribed her hormonal birth control pills. Doctors gave her forms about things that cause pelvic pain—conditions like STDs, fibromyalgia, and endometriosis. Nothing pointed to Essure. "Their findings didn't show anything wrong. How can you treat what's not wrong?" she says.
Elizabeth Fluegge, another Essure victim who needed to have her device surgically removed
Jessica returned to her gynecologist's office, where they couldn't find anything wrong, either. At one appointment, she says, her implanting physician's partner "accused me of being a pill seeker and said it's not possible for Essure to hurt because it's so small." In the same breath, however, Jessica says the doctor told her that, unlike her partner, she does not implant Essure, "because leaving metal in soft tissue is not a good idea.'"
The retailer where Jessica works initially denied her paid sick leave but then gave her the days retroactively, allowing her to support herself and her children on the days that she was in too much pain to work. Jessica eventually realized that the pain was at its worst during the time in her cycle when she was ovulating and when she was menstruating.
A year later Jessica found what she believed would be a long-term solution to her pain: a relatively unknown surgery called "Essure reversal." So-called Essure reversals are expensive, complicated procedures performed by fertility doctors; they're not covered by insurance. They promise the woman the chance to get their Essure removed from their body without undergoing a drastic hysterectomy procedure. What's more, doctors who perform Essure reversals say that women who previously had Essure may even be able to get pregnant again.
Jessica chose a doctor in Florida, who charged $6,000 for the procedure. "He said a third of his patients get pregnant afterward," Jessica says. Jessica's fiancée took out a medical loan from a financial firm the doctor conveniently provided a link to on his website. Initially the surgery seemed to cure her pain.
But the relief didn't last, and the pain returned. "It would be kind of intermittent, and then the periods of pain would be longer and longer until I was just in pain all the time again," she says.
In Austin, Jessica visited a new doctor—one who has become popular with Essure patients for offering them advice on Facebook and setting aside time at his practice to meet with them. When he examined Jessica, she says, she was in so much pain he warned her that he may not be able to help. "There isn't a recognized safe method to remove Essure," Jessica says. "So basically it's just doctors making stuff up without much oversight or regulation or anything."
The doctor told her he could remove the scar tissue causing her pain, but that it may grow back, and if it did, she would need to see a different doctor to perform the next, more technically complicated surgery. Jessica took the gamble and underwent her second post-Essure surgery with him anyway.
Jessica's ovaries, the doctor's report explained, were attached to her pelvic side walls, and "her right ovary [had] a significant attachment to the colon.
"The patient, upon inspection of the pelvis, had extensive adhesive disease of the colon and small bowel... she also had severe pelvic disease from the top of fundus down to the endocervix," reads the doctor's surgical report, which Jessica saved. Jessica's ovaries, his report explained, were attached to her pelvic side walls, and "her right ovary [had] a significant attachment to the colon."
This surgery, like the last, only gave Jessica temporary relief. In pain and missing more work again, Jessica searched for another doctor and found one who still implants Essure in women but who also took her pain seriously.
On March 22, she scheduled her third post-Essure surgery. Beforehand, her doctor told her he would not perform a hysterectomy unless it was absolutely necessary.
"Out of surgery," Jessica texted me the next day. "I had a hysterectomy. "They took my uterus, cervix and tubes. I'm sad... This is not what I wanted. We are still paying for my reversal."
Her doctor had found so much scar tissue that he had little choice but to remove much of her organs. "He told me that Essure works very well for most women. Just not for me," she says. "'And 28,000 other women,' I said, because I am relentless."
Now Jessica is recovering and hoping to return to work. She recently busted a stitch open in her belly button after hiding Easter eggs with her children, but says it's otherwise going okay. She still has her job and is waiting for word on if her disability leave will be covered during her recovery time. In the meantime, she has joined a lawsuit against Bayer AG. Though the company's special FDA approval bars it from lawsuits, attorneys are attempting to sue the company anyway, and they recently won a surprising, minor success from a judge who allowed two claims against the company to go forward.
 Jessica also leans on her friends for support. Her two friends and coworkers who sat in the interview with her have taken her to the hospital or watched her children when she was in too much pain to stand. And, in an effort to help Jessica with her medical bills, they even organized a surprise fundraiser last month, complete with a band and dozens of vendors at a local bar. The name of their event, written out in all-caps on the marquis of the bar, summed up the attitude that Jessica has about the last past two years of her life: "FUCK YOU, ESSURE."
Jessica also leans on her friends for support. Her two friends and coworkers who sat in the interview with her have taken her to the hospital or watched her children when she was in too much pain to stand. And, in an effort to help Jessica with her medical bills, they even organized a surprise fundraiser last month, complete with a band and dozens of vendors at a local bar. The name of their event, written out in all-caps on the marquis of the bar, summed up the attitude that Jessica has about the last past two years of her life: "FUCK YOU, ESSURE."