http://fortworth.legalexaminer.com/medical-devices-implants/depuy-pinnacle-hip-replacement-lawsuits-back-to-trial-in-texas/New Jersey and New York residents are the plaintiffs3:11-cv-02460Kathleen Riedhammer | 3:12-cv-04647Claudia and Alan Heroth | 3:13-cv-00244Susan H. Cousin | 3:13-cv-04119Hazel Miura | 3:14-cv-01776Michael A and Audra L Stevens | 3:14-cv-02341Eugen Jr. and Yolanda Stevens | 3:14-cv-02750Denise Buonaiuto | 3:15-cv-03489Ramon and Carole Alicea | 3:16-cv-01245Uriel and Aviva Barzel | 3:16-cv-01526Karen Kirschner
Joint replacements are the #1 expenditure of Medicare. The process of approving these medical devices is flawed according to the Institute of Medicine. It is time for patients' voices to be heard as stakeholders and for public support for increased medical device industry accountability and heightened protections for patients. Post-market registry. Product warranty. Patient/consumer stakeholder equity. Rescind industry pre-emptions/entitlements. All clinical trials must report all data.
Please share what you have learned!
Twitter: @JjrkCh
Showing posts with label metal toxicity. Show all posts
Showing posts with label metal toxicity. Show all posts
Tuesday, August 29, 2017
September 5, 2017: J&J Depuy Pinnacle hip fourth bellwether Dallas, Texas Federal jury trial begins
Labels:
DePuy,
J&J,
JNJ,
metal on metal hip implant,
metal toxicity,
NJ,
NY,
product design defect,
product liability
Dallas, TX, USA
Dallas, TX, USA
Friday, November 4, 2016
Harmed Patients Given Unjust Solomon's Choice: Trust the Settlement is Best Option or Jury Trial
Additional information:
http://www.pmkm.com/plaintiffs-leadership-counsel-announce-a-settlement-program-for-wright-medical-metal-on-metal-hip-implants/
PART 1
Plaintiffs’ Leadership Counsel Announce a Settlement Program for Wright Medical Metal-on-Metal Hip Implants
Anthonia Spencer | November 2, 2016
After a hard-fought, almost 5-year battle in federal court in Atlanta, Georgia and in California state court, we are pleased to announce a settlement program that will resolve a significant number of claims against Wright Medical. Wright Medical has agreed to settle approximately 1,300 claims of certain Wright Medical metal-on-metal hip implant patient-claimants whose hips were revised at least 150 days and no more than eight years post-implant. There are approximately 2,300 pending claims involving Wright Medical’s Conserve, Lineage, and Dynasty metal-on-metal hips. Plaintiffs’ Leadership Counsel’s retained financial analysts have been evaluating Wright Medical’s ability to settle these cases for years. Based on that analysis, we believe that Wright Medical was not in a position to and therefore could not agree to settle the remaining claims involving revisions occurring after eight years or other cases that it deemed not qualified at this time. During the negotiations with Wright Medical, it was made clear that claims for revised Wright metal-on-metal hips that are not included in this settlement will be part of subsequent settlement programs.
The Wright Conserve Multi-District Litigation (MDL) was consolidated in February 2012 in federal court in the Northern District of Georgia before the Hon. William S. Duffey, Jr., United States District Judge. Additionally, a Judicial Council Coordination Proceeding (JCCP) petition was approved in May 2012 before the Hon. Jane Johnson, Los Angeles Superior Court Judge, consolidating California state-court cases involving Wright Medical hip replacement and revision matters, including Wright Medical’s Conserve, Lineage, and Dynasty hip implants. The Hon. Diane M. Welsh (Ret.), led the extended settlement negotiations and tirelessly worked with the parties for several years to help facilitate the settlement.
Wright Medical’s hip and knee division (OrthoRecon) was sold in January 2014, and the successor corporation has a defense that it did not inherit the liability. Our financial analysts’ review further indicated that Wright Medical’s ability to fund this settlement depended largely on insurance coverage and a bond issue used, in part, to raise money for this settlement. Wright Medical has been engaged in litigation in Memphis with most of its insurance carriers and recently finalized an agreement with 3 of the carriers. It remains in litigation or coverage disputes with its remaining carriers. In light of our analysis of Wright Medical’s financial condition, this is a timely and meaningful settlement, offering $170,000 to claimants who had the monoblock Conserve Cup, the device with the most frequent failures, and $120,000 to those who had the metal-liner Dynasty and Lineage devices. An additional, but capped, limited fund is also available for claimants who suffered discrete and defined claims of extraordinary injury. More importantly, the settlement program calls for pre-qualification, without registration, coupled with a very simple administrative process for claimants not pursing extraordinary injury claims that will lead to expeditious payments expected to be largely complete by summer 2017. Counsel for eligible claimants will be notified of their pre-qualification by February 3, 2017.
Plaintiffs’ Leadership Counsel consists of Michael L. McGlamry of Pope McGlamry, P.C. in Atlanta, Georgia, mmcglamry@pmkm.com / 404-523-7706; Raymond P. Boucher of Boucher LLP in Woodland Hills, California, ray@boucher.la / 818-340-5400; Helen Zukin of Kiesel Law in Beverly Hills, California; Peter Burg of Burg Simpson in Englewood, Colorado; Christopher Yuhl of Yuhl Carr, LLP in Marina del Rey, California; Sean Jez of Fleming Nolen & Jez, L.L.P. in Houston, Texas; and Ellen Relkin of Weitz & Luxenberg, P.C. in New York, New York.
http://www.pmkm.com/plaintiffs-leadership-counsel-announce-a-settlement-program-for-wright-medical-metal-on-metal-hip-implants/
PART 1
Wright Medical Group to settle over metal-on-metal hip implants for up to $240M: 5 things to know
Amsterdam, Netherlands-based Wright Medical Group entered into a Master Settlement Agreement over litigation on its Hip Implant products.
Here's what you need to know.
1. Wright and the lawyers representing the plaintiffs agreed to settle 1,292 revision claims concerning its Conserve, Dynasty or Lineage hip implants
2. Wright will settle for up to $240 million with $180 million in cash and $60 million for insurance recoveries.
3. The settlement requires a 95 percent opt-in clause. Wright Medical will void the settlement if more than 5 percent of the plaintiffs opt out of it.
4. CEO Robert Palmisano said he was pleased to reach the settlement, and the company will now focus on "accelerating growth opportunities in its extremities and biologics markets."
5. Wright will "vigorously defend" any claims that were not settled. The company estimates there are 600 cases that will not be included in the settlement.
http://www.beckersspine.com/orthopedic-spine-practices-improving-profits/item/34049-wright-medical-group-to-settle-over-metal-on-metal-hip-implants-for-up-to-240m-5-things-to-know.html
PART 2:
Wright Medical Group N.V. Announces Entry Into Metal-On-Metal Hip Litigation Settlement AgreementPreviously Disclosed Agreement In Principle with Three Insurance Carriers Also Finalized Settlement In Line with Previously Disclosed Range of Loss
AMSTERDAM, The Netherlands, Nov. 02, 2016 (GLOBE NEWSWIRE) -- Wright Medical Group N.V. (NASDAQ:WMGI) today announced that on November 1, 2016, its wholly owned subsidiary Wright Medical Technology, Inc. (WMT) entered into a Master Settlement Agreement (MSA) with Court-appointed attorneys representing plaintiffs in the previously disclosed metal-on-metal hip multi-district litigation known as In Re: Wright Medical Technology, Inc., CONSERVE® Hip Implant Products Liability Litigation, MDL No. 2329 (MDL) and the consolidated proceeding pending in state court in California known as In re: Wright Hip System Cases, Judicial Council Coordination Proceeding No. 4710 (JCCP). In addition, on October 28, 2016, the Company entered into a Settlement Agreement with three of its insurance carriers (Three Settling Insurers).
Under the terms of the MSA, the parties agreed to settle 1,292 specifically identified CONSERVE, DYNASTY or LINEAGE revision claims which meet the eligibility requirements of the MSA and are either pending in the MDL or JCCP, or are subject to tolling agreements approved in the MDL or JCCP, for a total settlement amount of $240 million, of which approximately $180 million will be funded from cash on hand and $60 million will be funded from insurance recoveries.
Eligibility requirements of the MSA include that the claimant has a pending or tolled case in the MDL or JCCP, has undergone a revision surgery within eight years of the original implantation surgery, and that the claim has not been identified by WMT as having possible statute of limitation issues. Claimants who have had bilateral revision surgeries will be counted as two claims but only to the extent both claims separately satisfy all eligibility criteria.
The MSA includes a 95% opt-in requirement, meaning the MSA may be terminated by WMT prior to any settlement disbursement if claimants holding greater than 5% of eligible claims in the Final Settlement Pool elect to “opt-out” of the settlement. No funding of any individual plaintiff settlement will occur until the 95% opt-in requirement has been satisfied or waived.
Robert Palmisano, president and chief executive officer, commented, “We are very pleased to have reached this settlement agreement, in particular the population of claims that the settlement covers as well as the required 95% opt-in rate for those claims. With this clarity, we will continue to focus on accelerating growth opportunities in the extremities and biologics markets. This settlement addresses approximately 85% of the known U.S. revision claims that do not have potential statute of limitations issues and removes a great deal of the uncertainty that has been associated with this litigation.”
Wright will continue to vigorously defend metal-on-metal hip claims not settled pursuant to the MSA. As of September 25, 2016, the company estimates there were approximately 600 outstanding metal-on-metal hip revision claims that would not be included in the MSA settlement, including approximately 200 claims with an implant duration of more than eight years, approximately 300 claims subject to possible statute of limitations preclusion, approximately 30 claims pending in U.S. courts other than the MDL and JCCP, approximately 50 claims pending in non-U.S. courts, and approximately 20 claims that would be eligible for inclusion in the settlement but for the participation limitations contained in the MSA. The company also estimates that there were approximately 700 outstanding metal-on-metal hip non-revision claims as of September 25, 2016. These non-revision cases are excluded from the MSA.
The final MSA settlement amount (not to exceed $240 million), and the final number of claims settled under the MSA, will depend on, among other things, the number of claimants electing to participate in the settlement and the mix of products implanted in the settling claimant group. Claims which do not meet the eligibility requirements of the MSA, new claims, and claims which have opted-out of the settlement will not be settled under the MSA and the company will continue to defend these claims.
The company previously disclosed a loss range applicable to a substantial portion of revision cases of $150 million to $198 million and, in accordance with U.S. generally accepted accounting practices (US GAAP), recognized as a charge within discontinued operations in the second quarter of 2016 $150 million, the low end of the range of probable loss for these cases. During the third quarter of 2016, the company recorded charges of approximately $39 million to increase its accrual from the low end of its previous range of probable loss to the amounts in line with the final agreements and to record accruals for certain other revision cases. Please refer to the disclosures in the company’s third quarter 2016 quarterly report on Form 10-Q for a full discussion of our accruals and disclosures related to this matter.
WMT has agreed to escrow $150 million to secure its obligations under the MSA, and parent corporation Wright Medical Group N.V. has agreed to guaranty WMT’s obligations under the MSA.
The MSA will help bring to a close significant metal-on-metal litigation activity in the U.S. Some lawsuits, however, will remain and Wright will continue to defend against remaining claims and any future claims that could be filed. The ultimate cost to entirely resolve these matters will depend on many factors that are difficult to predict and may be materially different than the amounts accrued to date, including future revision claims and additional insurance recoveries. Further charges may need to be recorded in the future as additional information becomes available.
Internet Posting of Information
Wright routinely posts information that may be important to investors in the “Investor Relations” section of its website at www.wright.com. The company encourages investors and potential investors to consult the Wright website regularly for important information about Wright.
About Wright Medical Group N.V.
Wright Medical Group N.V. is a global medical device company focused on extremities and biologics products. The company is committed to delivering innovative, value-added solutions improving quality of life for patients worldwide and is a recognized leader of surgical solutions for the upper extremities (shoulder, elbow, wrist and hand), lower extremities (foot and ankle) and biologics markets, three of the fastest growing segments in orthopaedics. For more information about Wright, visit www.wright.com.
™ and ® denote trademarks and registered trademarks of Wright Medical Group N.V. or its affiliates, registered as indicated in the United States, and in other countries. All other trademarks and trade names referred to in this release are the property of their respective owners.
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
This release includes forward-looking statements under the Private Securities Litigation Reform Act of 1995. These forward-looking statements generally can be identified by the use of words such as “will,” “may,” “continue,” “anticipate,” “expect,” “could,” “believe,” “estimate,” “future,” other words of similar meaning and the use of future dates. Forward-looking statements in this release include, but are not limited to, statements about the effects of the settlement agreements and the amount and funding of the settlement amounts. Forward-looking statements by their nature address matters that are, to different degrees, uncertain. Each forward-looking statement contained in this release is subject to risks and uncertainties that could cause actual results to differ materially from those expressed or implied by such statement. Applicable risks and uncertainties include, among others, risks and uncertainties associated with the MSA and the settlement agreement with the Three Settling Insurers, including without limitation, the final MSA settlement amount and the final number of claims settled under the MSA, the possibility that the 95% opt-in requirement may not be achieved, the resolution of the remaining unresolved claims, the effect of the broad release of certain insurance coverage for present and future claims, the resolution of the company’s dispute with the remaining carriers; and the other risks identified under the heading “Risk Factors” in Wright’s Annual Report on Form 10-K for the year ended December 27, 2015 filed by Wright with the SEC on February 23, 2016 and Wright’s Quarterly Report on Form 10-Q for the quarter ended September 25, 2016 anticipated to be filed by Wright with the SEC on November 2, 2016. Investors should not place considerable reliance on the forward-looking statements contained in this release. Investors are encouraged to read Wright’s filings with the SEC, available at www.sec.gov, for a discussion of these and other risks and uncertainties. The forward-looking statements in this release speak only as of the date of this release, and Wright undertakes no obligation to update or revise any of these statements. Wright’s business is subject to substantial risks and uncertainties, including those referenced above. Investors, potential investors, and others should give careful consideration to these risks and uncertainties.
Investors & Media:
Wright Medical Group N.V.
Julie D. Tracy
Sr. VP, Chief Communications Officer
(901) 290-5817 (office)
Wright Medical Group N.V.
http://ir.wright.com/phoenix.zhtml?c=129751&p=irol-newsArticle&ID=2218769
Labels:
adverse event,
confidentiality agreement,
defective product,
discovery,
Eric Oliver,
gag clause,
metal on metal,
metal toxicity,
patient harm,
revision surgery,
Robert Palmisano,
verdict,
Wright Medical Group
Dallas, TX, USA
Amsterdam, Netherlands
Thursday, October 15, 2015
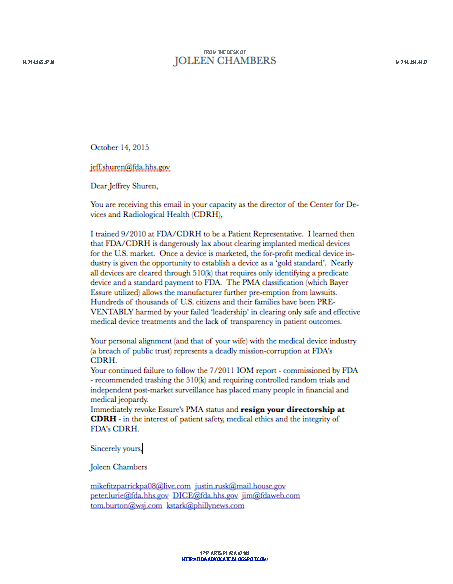
Call for Resignations of FDA/CDRH Directors Shuren and Maisel
Allison Shuren, wife of FDA/CDRH Director
William Maisel, FDA/CDRH Deputy Director
PREVENTABLE Patient Harm from lax FDA/CDRH regulation
Metal-on-metal hips 500,000
Pelvic Surgical mesh 70,000
Bayer Essure 20,000
Power Morcellator for pelvic surgeries
Duodenoscope infections
Bard 'Recovery' Blood Clot Filter fatalities
Labels:
510(k),
adverse events,
Allison Shuren,
Bayer,
CDRH,
Essure,
FDA,
Jeffrey Shuren,
metal toxicity,
metal-on-metal hip,
pelvic surgical mesh,
William Maisel
Dallas, TX, USA
Silver Spring, MD, USA
Sunday, August 23, 2015
New Zealand: Stryker strikes out with FAILED metal hips!
One woman's toxic surgery ordeal
9:55 AM Saturday Aug 22, 2015
David Fisher is a senior reporter for the NZ Herald.
Lynne McKay had both her hips replaced in 2007 with metal implants.
• The implants failed, causing her intense physical pain and violent mood swings.
• When the implants were eventually removed in 2012, a company representative attended the surgery and took photographs.
• A Health and Disability Commission investigation found no fault with McKay's medical care.
• About half the 5,000 metal hip implants given to New Zealanders have proved defective in some way but follow-up is left to the companies and surgeons involved.
• The implants failed, causing her intense physical pain and violent mood swings.
• When the implants were eventually removed in 2012, a company representative attended the surgery and took photographs.
• A Health and Disability Commission investigation found no fault with McKay's medical care.
• About half the 5,000 metal hip implants given to New Zealanders have proved defective in some way but follow-up is left to the companies and surgeons involved.
"When I licked my lips I could taste metal," says Lynne McKay, who has had six hip replacements in six years. "There was a metallic film on top of the water in the toilet and I was having to clean it every day. I was peeing [metal] ions."
The new life she expected to come with her double hip replacement in 2007 never arrived. Instead came fears of madness and near-constant misery, which only partly abated when the metal hips were removed after being recalled as faulty in 2012.
The time in between was awful. Almost immediately, there was pain. Inside McKay's body, the connection between the ball and the cup created a "grinding" which produced an "ionic soup".
When McKay walked, she heard "click, click" as the ball ground against the edge of the cup. Unknown to her, there were "actual chips coming off the back. And the [metallic] dust". The joints - when they eventually came out - were abraded, ground and scratched.
Her body was "trying desperately to sort it out" by collecting the metal fragments into tumours around the hip area. "There was a tumour the size of a small hen's egg."
Then came other changes. "About two years after having my hips done, in hindsight, I started to experience toxicity."
McKay had yellow, green and blue curtains, which first dulled, and then lost their yellow tones. At first she thought the curtains were fading, then she realised she was losing her ability to see colours. She started to experience hearing loss and tinnitus, and had frequent unexplained rashes.
McKay thought she was losing her mind. "I couldn't hold a thought. I was always in tears. My words weren't coming out right. I was cutting my nose off with all my friends. I thought I had Alzheimer's. I really thought I was losing the plot."
With her life falling apart, McKay tried harder to keep it together. She walked the streets for hours doing letterbox drops to build a massage business, which was suffering. "I was desperate for work. I was begging people. I really lowered my professional life. I was fighting for my life on a lot of different levels without knowing what was going on."
Understanding arrived in 2012, when the Stryker Mitch THR (total hip replacement) System was subject to a recall notice. A blood test showed McKay had high levels of chromium and cobalt in her bloodstream. Normal levels are between zero and 20 microscopic nanomoles per litre. McKay had 326 nmol/l. Cobalt was also high - safe was 0-16 nmol/l but she had a 378 nmol/l reading.
Mackay believes her metal hips poisoned her. It's a belief shared by other implant patients with elevated cobalt and chromium readings. The British Medical Journal raised this in 2012 in a story on regulatory failure around metal-on-metal implants, saying the ongoing uncertainty around the impact of the metal ions would never be tolerated in drug regulation.
There is still argument in medical circles as to whether the high levels have any effect, even though concerns have been raised for more than 40 years. The official position is that the long-term effects are unknown.
For McKay, not knowing is unacceptable. She says efforts should be made to find out the effects of metal ions in her body, rather than adopting a "wait and see" approach.
But then, she's long lost faith that the medical system will listen to her.
Back when she was a believer, the former registered nurse anticipated life-changing results from the metal hips surgeon Rocco Pitto put into her body during surgery at Middlemore hospital in 2007.
She was 50 at the time and life had become increasingly painful. "I got to a place where I could only walk to the letterbox with two walking sticks."
Diagnosed with dysplasia, a condition in which abnormal growths form at the joints, she had both hips replaced in March 2007. In hip replacements, the femur is removed for an artificial replacement; in McKay's case, the metal stem was attached to a metal ball that moved inside a metal cup, mimicking the worn-out original.
The metal hip replacements were enjoying a resurgence in surgical popularity, with the belief they would be more durable and last longer than ceramic or plastic alternatives. But by 2010, concerns were raised widely about the safety of metal-on-metal with the recall of a DePuy-branded device.
In April 2012, the recall notice for McKay's device went out.
The Lancet medical journal raised the alarm with a study showing 6.2 per cent of implants had to be replaced five years after being put in. It compared to 2.3 per cent for ceramic-on-ceramic implants and 1.7 per cent for metal-on-plastic types. British figures showed McKay's implants - the Stryker Mitch THR System with an Accolade femoral stem - had a revision rate of 8.8 per cent over four years. The alert to surgeons in Britain included advice that they screen patients annually for the presence of chromium and cobalt in the body.
In New Zealand, documents released under the Official Information Act show Stryker initially wanted to class the notice as a "safety alert", saying it no longer distributed the device in New Zealand. Medsafe wrote back to say it did not agree and insisted the notice be classified as the more serious "hazard alert", effectively matching the British response.
The letter announcing the recall on the Mitch head went out to surgeons on April 13 2012. Under the New Zealand system, the state has no role to play in contacting surgeons.
Instead, the regulator - Medsafe - asks the medical device company to make contact with the surgeons to whom it sold the implants and for them to notify patients. The OIA papers show Stryker didn't hear back from all surgeons (who it calls "customers" in emails to Medsafe) who used the device until three months later on July 6 2012.

McKay believes her metal hips poisoned her. Photo / Jason Oxenham
In McKay's case, Pitto's recalls were handled through Middlemore Hospital. Furious at the impact on her life over the past five years, she says she developed strong feelings of anger and frustration towards Stryker.
She wanted to sue. She wanted justice: "I had asked for medical photographs to record the damage to my hip. The kids had started to tell me I needed to collect things for class action."
She wanted to get Stryker into court and sue the company for the grief it had caused.
When McKay went into surgery in July 2012, she says she had no knowledge of - and did not consent to - a Stryker representative being among the gowned and masked surgical team preparing to operate. She says she objected strongly and was even more upset on waking after surgery to see on her notes: "The representative of Stryker Medical was attending today's surgery and also took some photos."
McKay: "That's when I lost it. Those photos were my evidence of what had happened to me." The faulty parts were also removed.
Though Pitto later told a Health and Disability Commission investigation he did discuss consent with Ms McKay, the Counties-Manukau District Health Board has said he didn't need her permission to have a Stryker representative in surgery and didn't ask her. The board also told the Herald - and Ms McKay says it's the first she's heard - that the Stryker photographs were not of the surgery but only of the faulty parts, removed from her body. She can't see the images to assure herself - the board says Stryker has deleted the photographs.
There are no signed consent forms showing permission was granted for either Stryker's presence, or the company's decision to take photographs or for the removal of the faulty parts. In all those cases, the health board says no consent was needed. It says consent is not required when someone is part of a surgical team.
For McKay, it felt as if the system was aligned against her - and even aligned with the company she blamed for the faulty part
In the end, McKay had a further three operations - a total of four hip replacements in 13 months after the recall. The replacement of the first metal hip in July 2012 was a failure - it dislocated less than two months later and needed replacing in November 2012.
One foot after another, neither working properly, "I fought to keep moving," says McKay. The replacement hip went in backwards so was replaced again on May 29, 2013. And then it was the other side. The right hip was revised in August 2013 and she then went into recovery for a year, getting $257 a week from ACC with a small accommodation top-up. Now, at least, "the metal taste was gone and energy levels were back up. But I'm in constant pain." She hisses with frustration.
"I'm sick of saying that actually. I walk like a drunk woman. I've no sense of stability in my hips. It hurts me to walk upstairs. My body is managing the indiscrepancies in core balance muscles but I pay for it in other ways. The body reorganises itself around weak muscles.
"I'm back massaging but I have to do it differently. I do my gardening and my housework on my knees."
McKay doesn't want anyone's sympathy. She's angry with nothing to strike out at. A complaint to the Health and Disability Commission talked of the "benefit of hindsight" and said Pitto's professional practice was appropriate given the knowledge at the time. Pitto declined to speak to the Weekend Herald.
And that's it. The metal hips that went bad inside her body were never approved for use in New Zealand, because our system doesn't require approval for medical devices.
The surgery took place largely in public hospitals, paid for with public money, and the taxpayer has since supported her recovery with a (meagre) salary supplement. ACC has never kept track of how much it cost the public to cover surgery to replace defective products or to cover rehabilitation afterwards.
No public body is taking action to discover the extent of the issue and whether it could have been handled better. When a group of Kiwi patients set off to Britain courts to unsuccessfully sue Stryker for negligence, they did so without Government support.
A spokeswoman for the Counties Manukau District Health Board pointed to a Health and Disability Commission investigation which found "the care provided to Mrs McKay was appropriate in the circumstances.
The DHB acknowledges the distress and pain that Mrs McKay has suffered as a result of the metal on metal hip implant and apologises that she had to undergo further surgery to replace the device."
A spokeswoman for Stryker said the company had "strict policies" guiding the behaviour of its staff in and out of operating theatres and investigated any complaints against them. The company would not provide a copy of its policies and would not comment on the specific case.
The scale of the issue is difficult to gauge. A Medsafe briefing counted about 1200 metal-on-metal devices that were recalled or subject to hazard notices. A further 1300 metal-on-metal devices had failure rates so high that surgeons were advised to check on their patients regularly.
In some cases, the surgeons who carried out the operations have died or retired - Medsafe's hope is that their successors will reach out on their behalf.
Health Minister Jonathan Coleman's office hasn't had any briefings on the issue in the past two years.
A spokeswoman says the regulatory system worked as it was meant to - but that system is about to be completely overhauled. "Health care is always rapidly changing, including emerging technologies, and we need to look at how legislation can better support that."
A law for the new regulatory scheme is expected to be put before Parliament next year and will "regulate the quality, safety and efficacy/performance of all therapeutic products across development and manufacture, market entry, and use".
Among the patients given the 2500 implants that were never good enough, McKay and a small cluster of unknowns have had extreme adverse experiences.
"I worry about what the future holds after being toxic for so long," McKay says. "Sometimes you just have to suck it up and get on with it - but somebody should be accountable."
Implants approved before risk known
Metal hip implants were recognised as a risk to patients after they were approved for use, says a surgeon who advised the Australian Government on the technique.
Surgeon Peter Devane - a hip replacement and revision specialist - says metal implants and metal caps on affected joints grew in popularity through the 2000s although use varied around the world. New Zealand was more conservative than most.
Devane was part of the system that cleared the devices for use in Australia. Between 1998 and 2008 he sat on the orthopaedic committee of Australia's Therapeutic Goods Association, the body that advises government on which devices can be used. The Australian system approved products under guidelines developed by the Global Harmonisation Task Force, a collection of volunteer regulatory bodies and medical device companies from around the world. At the time, metal-on-metal hips were in the "2b" category which meant they faced few regulatory hurdles because they were considered to be a modification of a previously-approved product.
From about 2007, work began to upgrade the categorisation to reflect a higher risk, but metal-on-metal hips had already gone through. Devane says governments were left playing catch-up. A British Medical Journal article later labelled it regulatory failure.
In New Zealand, the use of the products peaked in 2007. "Then those reports on metal-on-metal started coming out. We were aware of them - regulatory bodies were aware of them. By 2010, metal-on-metal was down to 3 per cent (of hip replacements)."
The comparative low number of replacements here - about 5000 replacements - tempered the surgeons' responses. "We didn't want to create a panic culture because it's not as big a problem (as abroad)," says Devane.
New Zealand's regulator Medsafe doesn't have an "approval process". In a statement, it told the Herald: "The [New Zealand] legislation does not require any form of pre-market assessment of medical devices." Medsafe takes guidance from other regulatory authorities -including the TGA - while medical device companies sell direct to surgeons.
Medsafe has "no mandate to approve medical devices or to monitor their import into the country", the statement said. Instead, companies are obliged to register devices on a database. "A notification on the database does not signify that a medical device has been 'approved' in any way."
Labels:
510(k),
cobalt,
hip replacement,
metal toxicity,
New Zealand Herald,
patient harm,
Stryker
Dallas, TX, USA
New Zealand
Thursday, November 13, 2014
Friday, February 28, 2014
Tuesday, August 20, 2013
Is there proven value in high cost hip/knee implants?
Hospitals set supply cost-cutting targets, push
physicians to change behavior
Posted:
August 17, 2013 - 12:01 am ET
Tags:
Hospitals, Purchasing, Special Feature, Specialty Hospitals, Supply Chain, Systems, Top Stories
Patients
with a new cardiac pacemaker have an advantage over patients who have received
standard pacemakers: they can undergo MRI scans as a part of their care without
the risk of adverse events.
But
the new device costs hospitals $1,300 to $3,000 more than a traditional
pacemaker and could cut into a hospital's margin because Medicare and other insurers pay the same rate for
implanting MRI-compatible pacemakers as they pay for the standard pacemakers.
From a clinical perspective, physicians are put in the position of having to
predict which patients are likely to need an MRI and should receive the new
pacemaker.
It's
one of many supply-chain decisions hospital administrators have to make where
they must weigh the benefits of a new technology—such as the fact that the new
pacemaker doesn't improve immediate outcomes for the patient but may have
additional benefits in the long term—against its higher costs.
These
executives face similarly difficult decisions to slash millions of dollars in
supply expenses each year. In the case of the MRI-compatible pacemaker, one
executive says his system likely will pay more for the new pacemaker when
appropriate and seek offsetting cost reductions elsewhere in the supply chain.
“It's
one of those things where to make the quality of life better for our patients,
we're going to incur new costs,” says William Mosser, vice president of
materials management at Franciscan Missionaries of Our Lady Health System in
Baton Rouge, La.
Facing declining revenue and
reimbursement, hospital systems across the U.S. are making it a priority to
sharply reduce spending on supplies including gloves, syringes and hip
implants. Supplies typically make up hospitals' second-largest expense, after
labor costs. Hospitals spent about $255 billion on supplies and nonlabor
services in 2011.
Budget
pressure has led to increased scrutiny of the costs, clinical outcomes and
utilization of products. Many hospitals are setting cost-reduction targets,
evaluating the effectiveness of their group purchasing organizations, and
pushing for better data and analytics on products to persuade physicians to
accept changes to the types of devices or supplies being purchased.
More
than 60% of the hospital supply-chain executives who participated in Modern Healthcare's 2013 Survey of Executive Opinions
on Purchasing said they were very satisfied or satisfied with
their primary GPO. About 40% were somewhat satisfied or not satisfied.
Meanwhile, 59% of respondents said their primary GPO was very effective or
effective in controlling costs; the remaining 41% said their main GPO was
somewhat effective or not effective.
Cost reduction, clinical integration
“Everyone
that we deal with at the hospital level today is focused on cost reduction and
clinical integration and managing
patients to outcomes with a bent toward resource reduction,” says John
Bardis, chairman, president and CEO of MedAssets, one of the nation's largest
GPOs.
But many hospital executives say there
are cultural and operational challenges that can slow these kinds of
cost-cutting initiatives.
One major factor is that physicians
often have relationships with particular medical device manufacturers or have
used certain devices for a long time and are resistant to changing to other
devices.
Another is that the higher costs of new technologies touted as improving
quality of care can set back savings efforts. And in many cases, there is a lack of validated clinical data that can definitively prove whether a
particular product yields better results for patients.
“The
biggest hurdle we have is there is not a consistent and large enough base of
validated evidence,” Mosser says.
Like
many other hospitals, Franciscan is undertaking an initiative to cut millions
of dollars in annual supply expenses as it faces the prospect of significantly
lower reimbursement rates in the coming years. The program, which it calls
Healthy 2016, aims to cut $165 million in operating expenses, including $31
million in medical and surgical supplies and purchased services, over the next
three years.
Related Content
Download
the 2013 Modern Healthcare Survey of Executive Opinions
on Purchasing charts.
Other
hospital systems have implemented cost-cutting initiatives similar to the one
at Franciscan. Over five years, Lahey Health, based in Burlington, Mass.,
plans to cut
$40
million out of the $300 million it spends each year on medical and surgical
supplies. BJC HealthCare, a 12-hospital system based in St. Louis, plans to
reduce its $850 million in annual supply spending by $54 million this year,
and it's seeking to cut out an additional $150 million over the next three
years.
“This
is a primary focus across the system, from the CEO down,” says Nancy LeMaster,
BJC's vice president of supply chain. “In the last three years, as the
reimbursement pressures have been getting tighter and tighter, people have
really started to see how this could impact us. We call (supply chain) a
sustainable advantage rather than just a back-office function.”
Hospitals are undertaking a number of
strategies, including standardizing the types of products clinicians use, optimizing appropriate
utilization by physicians, nurses and other staff, and continuing to negotiate
lower prices for supplies. Many but not all hospitals have value-analysis
teams in place.
Focus on physician preference
A
big area of focus is usually physician preference items, such as hip or knee implants as
well as stents and other cardiac rhythm management devices. These are some of the costliest purchases
hospitals make.
BJC is focused this year on reducing
costs associated with spine implants. “This is an area of focus where the pricing does not appear correlated to the
cost to manufacture and sell the product, but rather has historically been
based on what the market would bear,” LeMaster says in an e-mail. “The market
can no longer bear this level of pricing.”
The
system's strategy focuses on first achieving market-competitive pricing with
the spine vendors, and then taking on utilization management and possibly
standardization.
Franciscan
is supporting a clinical variation project led by chief medical officers at
its five hospitals in Louisiana that seeks to better align the clinical
protocols of spine surgeons. That could reduce the number of vendors of spine
surgery products the system works with, from about 20 now.
“Spine
surgeons across our health system do things differently,” Mosser says. “Some
might overutilize. Some might underutilize. Some might use generic products,
and others are using different types of techniques. Our chief medical officers
are working down a path of aligning both the protocols and the practices from
a clinical perspective that will allow us to minimize (the) number of those
vendors.”
GPOs
say their core business is still supply contracts, but the other services and
technologies they offer to hospitals to help address a number of financial
pressures are increasingly becoming of interest to their members.
“You've
got to look at best demonstrated practices,” says Ed Jones, president and CEO
of HealthTrust, a Brentwood, Tenn.-based GPO that is part of HCA's Parallon
Business Solutions. “You've got to look at reducing clinical variability.
You've got to look at streamlining your sourcing decisions.”
Nearly
half of the hospital supply-chain executives who participated in Modern
Healthcare's purchasing survey said they planned to increase their use of GPO
contracts in 2013. Only 7.6% said they planned to decrease their use of GPO
contracts.
“If
a big system feels like their GPO can give them access to scale and aligns
that scale to drive better value than they can do on their own, they will tend
to work more with the GPO,” Jones says. “If the larger systems are in a
position where their GPO is not as effective in that regard, they're probably
going to do it on their own.”
Smaller
health systems and hospitals are generally more inclined to work with GPOs and
increase their spending with them to gain the scale and volume that they
provide, Jones says. In other instances, contracts with higher commitment
levels also are generating more interest because they often deliver better
pricing, he adds.
Lahey
Health says it plans to review its current GPO relationships with Novation, a
GPO based in Irving, Texas, and MedAssets and then sign a contract in October
with a single GPO that will handle at least $180 million of spending.
“It's
a partner to help us meet our margin targets as we worry about declining
reimbursements,” says Eric Berger, Lahey's vice president of supply chain. “We
really need to look at expenses, so having a GPO partner will help us do that.”
Looking at the data
As
hospitals dive deeper into the supply chain searching for ways to reduce
spending, new areas of focus are emerging. Not only are some hospital systems
bringing distribution in-house, but they are also hiring new talent, investing
further in data and analytics tools, and some are even forming their own GPOs.
While
many hospitals report that they have met cost-reduction targets ahead of
schedule, the cost of
high-priced implants remains a big barrier. Hospital and GPO executives bemoan
that the implantables market has not become more like the markets for other
commodities.
“These innovations in total knee and
total hip have been around a long time but they've had a strong hold on high
prices compared to the rest of the world, in large part because of physician
relationships,”
MedAssets' Bardis says.
On
the other hand, teaching hospitals and physician-owned hospitals are more
likely to continue to allow preference among physicians. “We will tend to give
them what they want, regardless of what the cost is, in order for them to want
to practice there,” says Bruce Kizzier, director of materials management at
seven-bed Lincoln (Neb.) Surgical Hospital, a physician-owned hospital.
He
believes his hospital has gotten the best prices, noting that the hospital's
physicians have participated in meetings with vendors to ensure that the
hospital was receiving competitive pricing.
“More
organizations are having these conversations with surgeons,” says Dr. Peggy
Naas, an orthopedic surgeon and vice president of physician strategies for
VHA, the parent organization of Novation. “More surgeons, seeing the pressure
to add value, are asking questions.”
Other
supply-chain executives say that while hospitals have done a poor job in the
past in educating their physicians about the costs of preference items and
keeping supply costs under control, that's changing and doctors increasingly
are facing up to the problem.
“They've
seen the impact of the sequestration, the federal law changes and
reimbursement drops have been very dramatic across the country for every
system,” BJC's LeMaster says. “They're really seeing that if we don't get it
out of supplies, then we've got to look at labor.”
Read more: Hospitals push docs to change behavior to meet
cost-cutting targets | Modern Healthcare http://www.modernhealthcare.com/article/20130817/MAGAZINE/308179905#ixzz2cWhLwahv
?trk=tynt
Wednesday, June 12, 2013
Metal Allergy, Mother and Mystery: Joint Replacement Culprit
Christa Carmell Davis | Narratives
| Vol. 5, 2013 | June 5,
2013
Journal of Participatory Medicine (FiDA highlight)
Abstract
Summary: The author describes the detective work she did to find the
reason for her mother’s unexplained
deterioration and lack of muscular strength in hands and legs following joint
replacement surgeries. A careful neurological workup ruled out ALS but
did not result in a clear diagnosis. Her review of the medical literature
suggested that metal toxicity might be causing inflammation that was destroying
the muscle. She describes the numerous difficulties and eventual success she
had interacting with a number of physicians as her mother’s advocate.
Keywords: Participatory medicine, patient
engagement, inflammatory myopathy, metal allergies, joint replacements, muscle
weakness.
Citation: Davis CC. Steel standing: metal meets muscle;
a patient’s perspective. J Participat Med. 2013 Jun 5; 5:e23.
Published:
June 5, 2013.
Competing Interests: The author has declared that
no competing interests exist.
In 2008, my once active, vibrant,
and energetic 68-year-old mother began to lose her ability to do things
independently. Her body was succumbing to a debilitating weakness, and she was
rapidly becoming unable to feed, dress, or care for herself without assistance.
She had played the piano since
the age of 4, and been our church pianist for decades. Her upper body strength
was tremendous. Then the gradual onset of her weakness escalated. I began
noticing her difficulty in trying to pick up or hold a glass with both hands.
Previously, my mother had been
examined by a hand specialist who strongly suspected carpal tunnel because of
her history as a pianist and because her occupation before retiring included
typing on a computer keyboard for the majority of her work time. The results of
extensive testing and EEG were normal.
Within a few months of the onset
of trouble with her hands, however, weakness developed in her legs. Her primary
care physician referred her to a neurologist. The same tests and lab profiles
were repeated, in addition to an MRI. Still no resolution or clue was offered.
She appeared in good health with the exception of increasing muscle weakness, but
again nothing significant was evident.
Unless one knew my mother’s daily
behavior, actions, and habits, no one would have suspected she had troubling
health issues. She was never one to complain or express personal difficulties.
As her daughter, quickly becoming her primary caregiver, I also became her
walking diary. It was my
role as her spokesperson to communicate key information that my mother didn’t
think to share with her physicians.
In a few weeks, she was referred
to another neurologist with more clinical experience in a university (research)
setting. He was young, eager, and very intrigued by my mother’s odd
neuromuscular symptoms. After taking extra time to examine her carefully and
listen to the information I was able to offer from observing her on a daily
basis, he believed that she had ALS (Lou Gehrig’s disease). The next step was a
muscle biopsy. My mother gladly agreed. She was extremely eager to learn what
was happening with her body.
Within a few weeks she was
diagnosed with a myopathy. However, the diagnosis brought more questions to
mind, since a specific category of a myopathy or a potential cause was not
found. That’s when I began my own research.
At this point, I questioned: “Why
did the neurologist think mother had ALS and what were the symptoms he believed
were so closely associated with myopathy?” In studying ALS, I quickly
understood how the two conditions appeared closely related. Both started
slowly. However, the origin and outcomes of the overall muscle weakness for
each disease were quite different.
Hoping to learn which specific
myopathy she may have acquired, I did more in-depth reading and spoke with
close relatives about our family’s medical history. Based on this information,
it appeared likely that my mother had inflammatory myopathy. That diagnosis was
later confirmed by the neurologist who performed my mother’s muscle biopsy.
My next inquiry: “What could be inflaming her
muscles and when did it begin?” Inflammatory myopathy had six geneses
listed within its own category. There was only one that applied to my mother’s
medical case. It was metal toxicity. My mother had had a hip replacement due to
a fall in March 2006, followed by a knee replacement due to an injury 4 months
later in July 2006.
After days of trying to connect
her mysterious health issues, seemingly unassociated, I unearthed a 5-year
timeline while doing my taxes. Scribbled beside my mother’s surgery in 2006, I had written, “Her hands
became weak after her knee replacement.” This was a revelation!
Immediately, I acquired copies of
her medical records going back to 2005. Then I gathered information in talking
with her original orthopedic surgeon’s PA. If the metal in her knee was creating her weakness,
then I needed valid research to connect the dots of how the initial reaction
catapulted her once-healthy body into a spiral of decline. And now her
weakness was spreading; she could no longer walk without assistance. I needed
to link the research and present credible information and my theory to the
neurologist, with whom she would meet again in a few days.
As I continued specific research on metal implants, I uncovered a
wealth of medical information from European countries, with decades of clinical
studies presenting cases identical to my mother’s.[1] More specifically, the same
types of metals identified were also in my mother’s knee replacement; chromium,
cobalt and nickel. In some patient cases, the hypersensitivity to these metals was linked to
organ failure and possibly even cancer within five years.[2] Based on these reports, I
became convinced that if my mother’s knee replacement were to be changed to a
different type(s) of metal (we didn’t know at the time it was called a
“revision”), then her muscles would recover or at least stop deteriorating.
That was my theory.
In 2009, my idea was considered
farfetched. To my surprise, the neurologist at the university medical center
encouraged me to “go with your hunch.” He understood the premise of my
thinking. He knew her muscle tissues were dying based on the appearance of her
muscle biopsy. He urged us to seek her original orthopedist for further medical
care.
After mentioning possible “metal
toxicity” to the original orthopedic surgeon’s receptionist, we had an
appointment the next day. I armed myself with copies of the case studies I had
uncovered.
We arrived, fully equipped and ready to work with the orthopedist,
believing he would welcome the data and help my mother. She was the last patient to be called before the office closed
for lunch. The surgeon had always required an x-ray of my mother’s replacements
before seeing her. This time, we were escorted directly to the exam room. The
PA entered, leaving the door open.
The PA asked my mother why she
was there. She shared her symptoms of severe weakness and a clicking noise that
had just begun in her knee replacement. She stated that it felt loose when she
walked and how sore her knee had become in the past few weeks. The PA made
notes and exited.
In a few minutes, the surgeon
entered, again leaving the door open. He also questioned why my mother was
there to see him. She repeated her symptoms and he began an evaluation of her
knee. I held off presenting my theory and the evidence until I heard his
opinion.
He began his exam by pushing his
thumb on the area where the replacement stem connected below her knee. She
yelled, “OH that hurts!” My mother was never one to get above a normal voice
tone, much less shriek with agony. She was obviously hurting. The surgeon
continued to twist her knee from side to side. She again stated that he was
hurting her leg. Upon completion, he sat down on a stool and while looking
directly at my mother’s leg instead of her face, said, “I don’t think there is
anything wrong with her knee replacement.”
He certainly didn’t believe her
knee replacement and weakness were connected. He said it was normal to have
some pain and discomfort after some replacements, and they are rarely
pain-free. This was a stark contrast to their first discussion when he
explained how her bone-to-bone degenerative pain would be relieved with a knee
replacement. Since day one, she had pain with her knee replacement, sharing
this repeatedly with the surgeon.
My mother’s expression showed her
disappointment. She asked me to share my findings. I handed him several pages
of medical journals and other information. Although he had never heard of metal
allergies from a joint replacement, he seemed interested and appreciative as he
flipped through the pages. Then he asked me, “What do you want me to do? What
is the next step of action to take?” He was sincere, facing me as if I were a
medical colleague with answers to this crisis. I suggested my mother go to a
hospital for further testing as was done in the published studies. He pondered
the idea. He said he was concerned about the CPT billing code conflict. He
wasn’t sure how to admit her. He suggested we go to an ER, and have them call
him. I was stunned with his reaction. He stated that he didn’t know of any labs in the South
that could do metal allergy testing. He suggested the Mayo Clinic. I suggested
a knee revision!
He asked for us to wait while he
called a colleague and old college friend who did revisions. After almost an
hour, he returned with the name and phone number of his colleague, hand printed
on a sheet from his prescription pad.
We believed we were being referred to an orthopedic surgeon who was far
more advanced in revision surgeries and metal allergies. He was not.
When I called to schedule an
appointment, we were given the option of waiting either two days, or eight
weeks. We chose two days. The nurse on the other end of the phone curtly
demanded that we bring all of my mother’s medical records, x-rays, and any
other test results.
We arrived hopeful for solutions.
Within a short time my mother was called for a knee x-ray, after which we were
escorted to an exam room. Within a few minutes, the nurse told my mother to get
on the exam table and left her to perform this difficult task without any
assistance.
The surgeon entered about one
hour later. His demeanor was harsh, betraying skepticism before either of us
said a word. My mother tried to answer his questions as best she could. He
interrupted her remarks as if she were a witness for a prosecutor. It was
obvious this was not going nearly as well as we had hoped.
Jerking the exam table away from
a wall to get to her left knee, the surgeon pushed my mother down from a seated
position without any warning. He began applying pressure in what was evidently
a painful spot, while asking, “Is this where it hurts?” She screamed as tears
began to form in her eyes. He moved her knee from side to side as if it were a
piece of machinery and not connected to nerves, muscles, and bone. It was
obvious she was in pain, trying to hold back her tears. He had never asked about any details or symptoms.
It seemed he had already solved this medical mystery.
The surgeon finished his exam and
sat down, never helping my mother back to a sitting position. I rose from my
chair to help while she was struggling not to fall off the exam table. He proceeded
to the sink as if he were literally washing his hands of the entire ordeal. At
this point, my mother asked me to present my theory and evidence. Hesitantly, I
began to show him the data, sharing extra copies. He grabbed the papers from my
hands as if I had incriminating evidence. He asked me where I got my information. I answered, “On
the internet.” He said that was not a reliable source.
He exited the room fuming. For
the next few minutes, my mother and I quietly sat while waiting on his return.
We looked at each other bewildered.
When he returned, he informed us
that there was nothing wrong with my mother’s knee replacement. We didn’t try
to convince him otherwise. We left, as my mother limped in pain while leaning
on me.
We weren’t trying to blame anyone or seek legal action. My mother
needed help and quickly. One of our cousins is a family
practice physician. On the ride home, she called him to share her experience.
Our usually calm and gentle cousin was outraged. He said he would make
arrangements for her to see another orthopedic surgeon.
In a few days, she was again
examined. This orthopedic surgeon, although also skeptical, was willing to
consider a revision because of my mother’s apparent pain. He too denied any
possibility that her knee replacement had anything to do with metal allergies.
To keep a check on her labs, my
mother met again with her primary care physician. She shared her sorrowful
experiences. He suggested another orthopedic surgeon in the area.
Two weeks later, we met yet
another orthopedist, our fourth. This one was a subspecialist in adult joint
replacements. He had trained in hip resurfacing in Birmingham, England. He took
time to sit in the exam room with us as he read her medical records. He
reviewed her x-rays and bone scan. He immediately understood her condition, the
studies from Europe, and my theory. He said he was aware of metal allergies and
had performed revision surgeries due to metal allergies before. He looked at my
mother, asking one question, “When would you like to schedule a knee revision?”
The day of my mother’s knee
revision arrived and she was taken to the operating room. Four hours later, the
surgeon met with our family in a private room. He said, “It was a failed prosthesis. The metal never
adhered to her bone and muscle. The top part fell out into my hands and the
bottom part easily pulled out.” She had walked on a failed prosthesis for 37
months.
As her health began to stabilize
after this exhausting journey, my mother returned to the neurologist at the
university medical center for a followup visit.
In January 2011, he examined her
physical strength and believed her muscles had stopped deteriorating.
In February 17, 2012, my mother
returned for another followup. She passed the physical strength tests, showing
tremendous and much unexpected improvement. The neurologist examined her left
arm, where the original complicated muscle biopsy had left considerable
weakness, discovering her muscle tissue had begun to regrow and get back to its
baseline. He deemed her case
a non-clinical (only known case) medical breakthrough. At her next
appointment with the neurologist in January 2013, she greeted him with a
bear-hug, picking him up. He was elated.
Today my mother is driving, doing
household chores, active in social events, and plays the piano for community
occasions. “Steel Standing” is her true story which I penned to share an
unprecedented and compelling medical case, which correlates seemingly
unassociated health issues directly to metal allergies.[3]
References
1.
Keegan, G.M., Learmonth, I.D. and
Case, C.P. Orthopaedic metals and their potential toxicity in the arthroplasty
patient: A review of current knowledge and future strategies. Bone & Joint
Surg (Br) 2007; 89-B(5):567-573. ↩
2.
Keegan GM, Learmonth ID, Case CP.
A systematic comparison of the actual, potential, and theoretical health
effects of cobalt and chromium exposures from industry and surgical implants.
Crit Rev Toxicol. 2008;38(8):645-74. doi: 10.1080/10408440701845534. ↩
3.
Davis CC. Steel Standing
book website. Available at: http://www.steelstandingbook.com. Accessed June 3,
2013. ↩
Copyright: © 2013 Christa Carmell
Davis. Published here under license by The Journal of Participatory Medicine.
Copyright for this article is retained by the author, with first publication
rights granted to the Journal of Participatory Medicine. All journal content,
except where otherwise noted, is licensed under a Creative Commons Attribution
3.0 License. By virtue of their appearance in this open-access journal,
articles are free to use, with proper attribution, in educational and other
non-commercial settings.
Comments
2 Responses to “Steel Standing:
Metal Meets Muscle; A Patient’s Perspective”
.
Stephanie Miller says:
June
7, 2013 at 7:47 pm
Christa, thank you sharing your mother’s story. It bought tears
to my eyes. It’s a very powerful reminder of the importance of patient
engagement and the role of carers. Kind regards, Stephanie
Reply
chad lehan says:
June
10, 2013 at 9:39 am
Hello,
I have been battling the same issue with my wife. Only
her metal toxicity is cause from 11 cironary stents that can’t be removed.
Turns out if you can’t wear earrings because of a metal allergy, you shouldn’t
get ANY metal installed. It’s amazing the amount of denial doctors possess.
It’s not a new subject. Certainly WELL documented.
Subscribe to:
Posts (Atom)